- Cidpedia
- Posts
- "I Want A Cure"
"I Want A Cure"
Special Edition #5 –“I Want a Cure”
JULY 3 2025
🌟 Cidpedia Central Texas Resource
Trusted Information and Community for CIDP Patients, Caregivers, and Professionals
www.cidpedia.net

Broken not Shattered
Table of Contents
Editor’s Note: Deepening the Journey
Mock Research Team Update: Week 3—Scaling Up and New Challenges
Feature Article: Inside the Lab—A Day with the PPNRI Team
Team Spotlight: The People Behind the Science
Community Voices: Research and Resilience
Ask the Team: Your Questions, Our Answers
Resource Corner
Disclaimer-This is fictional

✉️ Editor’s Note: Deepening the Journey
Welcome back to our “I Want a Cure” series. As our Phoenix Peripheral Neuropathy Research Institute (PPNRI) team moves into Week 3 of their accelerated research timeline, the pace quickens. This issue takes you deeper into the daily work, the challenges, and the breakthroughs that define real-world CIDP research. Our team’s dedication and adaptability continue to inspire hope for patients and families alike.
This is all fictional and only for demonstration purposes.

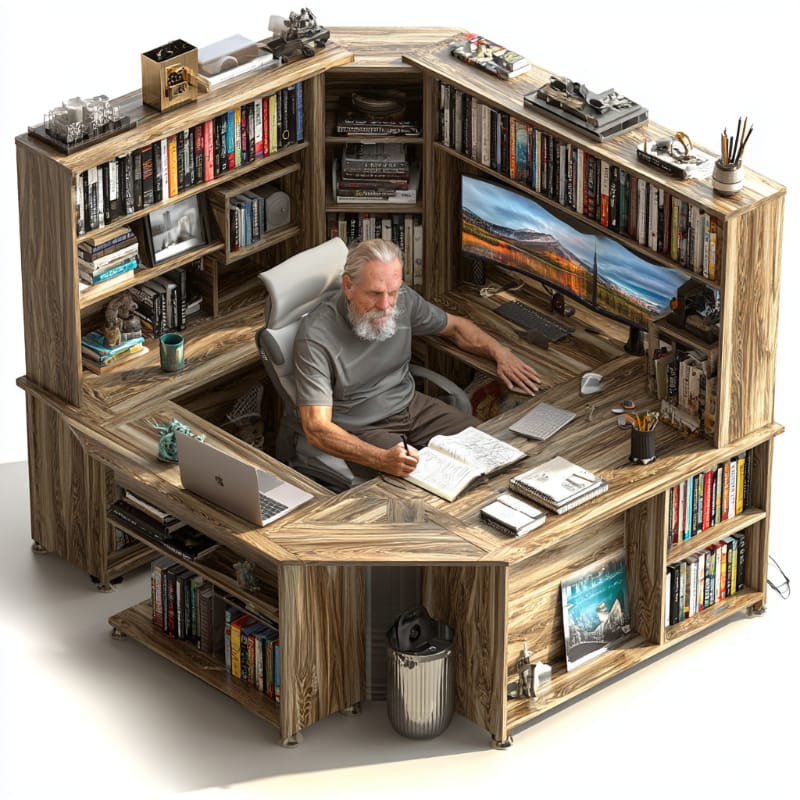
Buildout
🧬 Mock Research Team Update: Week 3—Scaling Up and New Challenges
The PPNRI team has expanded their volunteer cohort and begun testing new therapeutic approaches. Dr. Carter leads the charge in refining protocols, while Dr. Singh and Dr. Nguyen analyze growing datasets. Mr. Torres manages the increased lab activity, ensuring smooth operations, and Ms. Patel deepens patient engagement, gathering vital feedback.
Key developments include:
Increased volunteer recruitment to 40 participants, with diverse symptom profiles.
Introduction of a new subcutaneous immunoglobulin (SCIG) regimen trial.
Enhanced data integration techniques to correlate biomarker levels with clinical outcomes.
Implementation of remote monitoring tools to improve patient diary accuracy.

Startup
🔬 Feature Article: Inside the Lab—A Day with the PPNRI Team
Step inside the Phoenix lab at dawn, where the day begins with the soft hum of freezers and the gentle glow of incubator lights. Mr. Luis Torres arrives first, running a rapid systems check on the ultra-low temperature storage units and ensuring each sample’s digital log is intact. His steady hands and keen eye for detail prevent delays before a single pipette is lifted.
By 8:00 AM, Dr. Amara Singh greets the first volunteer of the day. With calm reassurance, she adjusts the nerve conduction electrodes and guides the participant through each pulse and measurement—her own CIDP journey lending empathy to every beep and blink of the monitor. “I know how unsettling those sensations can be,” she tells them, her voice as precise as the equipment she calibrates.
Meanwhile, Dr. Marcus Nguyen convenes his immunology team around the long bench. They review yesterday’s cytokine panel results, whiteboard arrows crisscrossing theories about unexpected spikes in anti-inflammatory markers. He pours over Simoa assay readouts, murmuring, “This pattern could hint at a new sub-group of responders,” as he annotates graphs with a Sharpie, the promise of discovery lighting his eyes.
In the corner, Ms. Sara Patel brings the human story forward. She meets families waiting for their appointments, translating consent forms into clear, compassionate dialogue. She listens as one volunteer recounts a weekend of joint pain and fatigue, logging these observations in the study database. “Your experience helps us refine every protocol,” she reminds them, turning raw data into meaningful insights.
As midday sun streams through the lab windows, the team breaks for a shared lunch—sandwiches and laughter weaving a moment of camaraderie amid the complexity. Dr. Carter drops by with updates on upcoming grant deadlines, reminding everyone that their meticulous work today fuels tomorrow’s breakthroughs.
Afternoon brings new challenges: a reagent batch fails quality control, prompting Mr. Torres to troubleshoot with engineering support; Dr. Singh pilots an adjusted stimulus protocol to improve signal clarity; Dr. Nguyen consults with a collaborator overseas on bioinformatics pipelines. Each setback is met with the same blend of scientific rigor and unwavering optimism that defines the Phoenix spirit.
When the lights dim late in the evening, the lab is still alive with quiet determination. Data files upload to the central server; consent forms are finalized for tomorrow’s volunteers; and a final round of equipment checks ensures the next day’s experiments begin without a hitch. Before leaving, the team gathers for a brief debrief—sharing one small triumph and one lingering question, knowing that these moments of reflection forge the path forward.
Every day in this lab is a testament to collaboration, compassion, and the relentless pursuit of a cure. Here, precision meets humanity, and each heart-felt interaction fuels the science that brings hope to the CIDP community.

Startup Again
🗣️ Community Voices: Research and Resilience
We asked: “What keeps you hopeful during your CIDP journey?”
“Knowing that every study brings us closer to better treatments.”
There’s a quiet hope that comes with every new research update. For many in our community, it’s the knowledge that each clinical trial, every new data point, and each patient story builds the foundation for tomorrow’s breakthroughs. Even when results aren’t immediate, just knowing that scientists are working tirelessly—testing new therapies, refining diagnostics, and learning from every setback—gives us a reason to keep going. It’s like watching a garden grow: sometimes progress is hidden beneath the surface, but with patience and care, we know something better is on the horizon. Every study is a step forward, not just for science, but for all of us waiting for relief and a brighter future.
“The support of the research team and fellow patients.”
Living with CIDP can feel isolating, but being part of a research study changes that. There’s comfort in knowing you’re not alone—whether it’s a nurse who remembers your favorite chair, a researcher who takes time to explain a test, or another patient who shares a similar struggle. The encouragement and understanding from the team and fellow participants becomes a lifeline. We celebrate each other’s small victories and offer a hand during setbacks. This sense of community, built on shared experience and mutual support, is as healing as any treatment. It reminds us that together, we are stronger, and that our voices and stories truly matter.
“Seeing progress, even if it’s slow.”
Progress in medical research is rarely fast, but every bit of improvement—no matter how small—feels monumental. Some days, it’s a new treatment option on the horizon; other days, it’s a slight increase in strength or a reduction in symptoms. Even when setbacks happen, the overall movement is forward. Watching the research team celebrate a successful data run or hearing about a new discovery gives us hope. It’s a reminder that change is happening, step by step. Slow progress is still progress, and every milestone brings us closer to the lives we want to reclaim.
“Being heard and involved in research decisions.”
One of the most empowering parts of participating in research is knowing our voices are valued. When the team asks for our feedback, listens to our concerns, and adapts protocols based on our experiences, it transforms us from subjects into true partners. It’s not just about being studied—it’s about shaping the study itself. This involvement builds trust and makes us feel respected and seen. When we’re invited to help design consent forms, suggest improvements, or share our daily realities, it ensures that research reflects what really matters to patients and families. Being heard isn’t just a courtesy—it’s a crucial part of making research meaningful and effective for everyone involved.

Proper Arrangement
❓ Ask the Team: Your Questions, Our Answers
Q: How do you manage the growing complexity of data?
A: Dr. Nguyen:
“As our study expands, the sheer amount of data we collect—from nerve conduction results to immune marker profiles and daily symptom diaries—can feel overwhelming. We rely on advanced analytics software that helps us organize, visualize, and compare thousands of data points in real time. But technology alone isn’t enough. Every week, our team gathers for what we call ‘data huddles.’ We sit around a table, project the latest charts on the screen, and talk through what we’re seeing. Sometimes a pattern jumps out—a cluster of patients with similar biomarker spikes, or a correlation between sleep quality and symptom flares. Other times, we debate and challenge each other’s interpretations. It’s this combination of digital tools and human collaboration that lets us turn raw numbers into real insights. We’re not just looking for statistical significance—we’re searching for meaning that can change patient care.”
Q: What’s the biggest challenge this week?
A: Dr. Carter:
“This week, our biggest challenge is striking the right balance between moving quickly and maintaining the highest standards of accuracy. With more volunteers joining and new protocols being tested, there’s pressure to process samples and analyze results as fast as possible. But every data point represents a person—a mother, a teacher, a friend—who is counting on us to get it right. That means double-checking every entry, confirming every lab result, and sometimes slowing down to investigate when something doesn’t add up. It’s tempting to rush, especially when hope is on the line, but we remind ourselves that a single error could set back months of progress. The stakes are high because lives are at stake. So, while we celebrate every milestone, we never lose sight of the responsibility we carry. Precision, patience, and teamwork are our watchwords this week.”
This is all fictional and only for demonstration purposes.
🧰 Resource Corner
GBS|CIDP Foundation International – Trials & support
ClinicalTrials.gov – Search CIDP studies
Shining Through CIDP – Patient stories
NeurologyLive CIDP Coverage – Latest news
📅 Closing Thoughts & How to Get Involved
Take advantage of these articles if you can, ask questions, and share what works for you. Together, we’re building a stronger, more informed CIDP community. |
To support Cidpedia.net |
Blaze you own trail, |
⚠️ Disclaimer |
Let's get something important out in the open: WE ARE NOT DOCTORS and WE ARE NOT GIVING ADVICE! Everything we share comes from my personal journey living with CIDP, from research and from MY healthcare TEAM. While I've walked this path for a number of years, please remember: This content is based on personal experience and publicly available information. It is not intended to diagnose, treat, cure, or prevent any disease. Always consult qualified healthcare providers for medical advice, what works for others may not work for you. |
We respect your privacy and adhere to HIPAA guidelines when sharing stories or community contributions. All shared experiences are anonymized unless explicit permission is granted |

Stay strong, stay curious, and keep shuffling forward. 🌱 |
Reply