- Cidpedia
- Posts
- Cidpedia "I Want A Cure"
Cidpedia "I Want A Cure"
I Want A Cure ISSUE #2 6/14/2025
🌟Empowering Central Texas
ALWAYS FRESH - Start your week empowered - updates, resources, and encouragement await!
Trusted Information and Community for Patients, Caregivers, and Professionals
www.cidpedia.net

Neurographic
Editor’s Note: While doing research for this series of articles, in a way, I hate what I found. Overnight cures don’t just happen and the average “cure” timeline for most diseases is very long.
BUT: don’t despair, we have research, we have trials, we have medical professionals working FOR US. Take heart and let’s see just how it all starts. Being educated is the best medicine.

I Want a Cure
When I was first diagnosed with CIDP, the words that echoed in my mind weren't about treatments or management — they were simple and desperate: "I want a cure." If you're reading this, chances are you've felt that same longing, that ache for your old life back, for strength that doesn't waver, for a body that doesn't betray you 123.
The truth about CIDP and the word "cure" is more complex than we'd like, but it's also more hopeful than you might think. Let me walk you through what the latest research tells us about our disease, what "cure" really means in CIDP terms, and why there's genuine reason for optimism in 2025.
What Does "Cure" Actually Mean for CIDP?
In medical terms, a cure means complete elimination of disease with no possibility of return 45. For CIDP, we don't have that kind of cure yet. But here's what we do have that's pretty remarkable: remission rates that would have seemed impossible just decades ago 46.
Doctors define CIDP remission in two ways. Complete remission means you're off all treatment for more than five years with normal nerve tests and no symptoms 7. Partial remission means you're living independently, maybe needing occasional treatment, but functioning well 78. When researchers followed CIDP patients for five years or more, here's what they found: about 15% achieved complete remission, and 47% achieved partial remission 96.
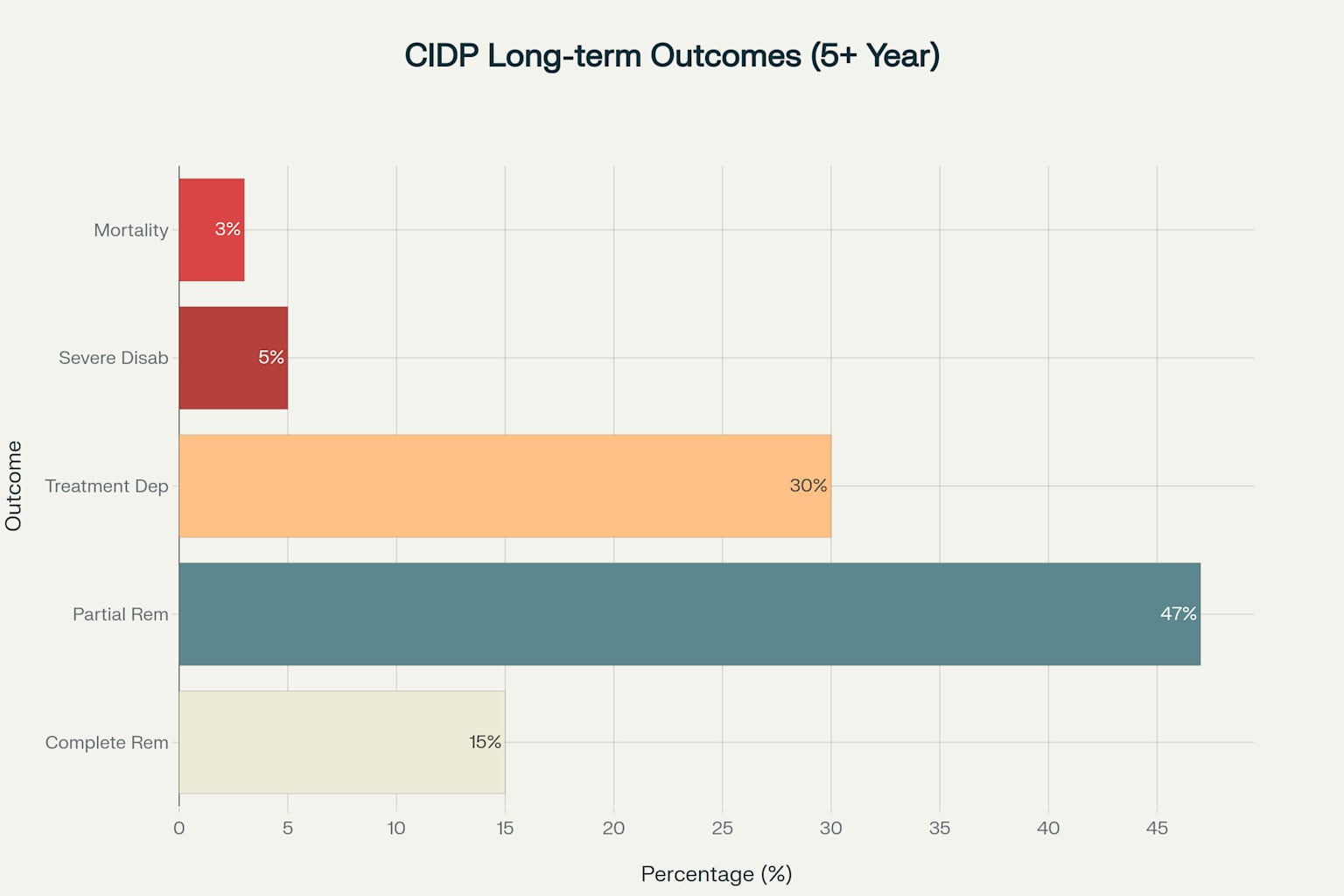
CIDP Long-term Outcomes: What the Research Shows About Recovery
That means nearly two-thirds of people with CIDP can expect to live independently with good function—and some will be completely medication-free 46. While this isn't the instant cure we dream of, it's a kind of healing our predecessors could barely imagine.
Today's Treatment Landscape: Better Than Ever
The treatment options available today represent genuine breakthroughs, especially when we catch CIDP early 10114. The three pillars of CIDP treatment—IVIG, corticosteroids, and plasma exchange—each help about 70% of patients, with about 26% achieving complete remission with IVIG or steroids 12137.
2024 marked a watershed moment for our community 1011. For the first time in over 30 years, the FDA approved a completely new type of CIDP treatment: efgartigimod (Vyvgart Hytrulo) 11. This weekly injection works differently than anything before it, blocking specific immune pathways and reducing relapse risk by 61% compared to placebo 11.
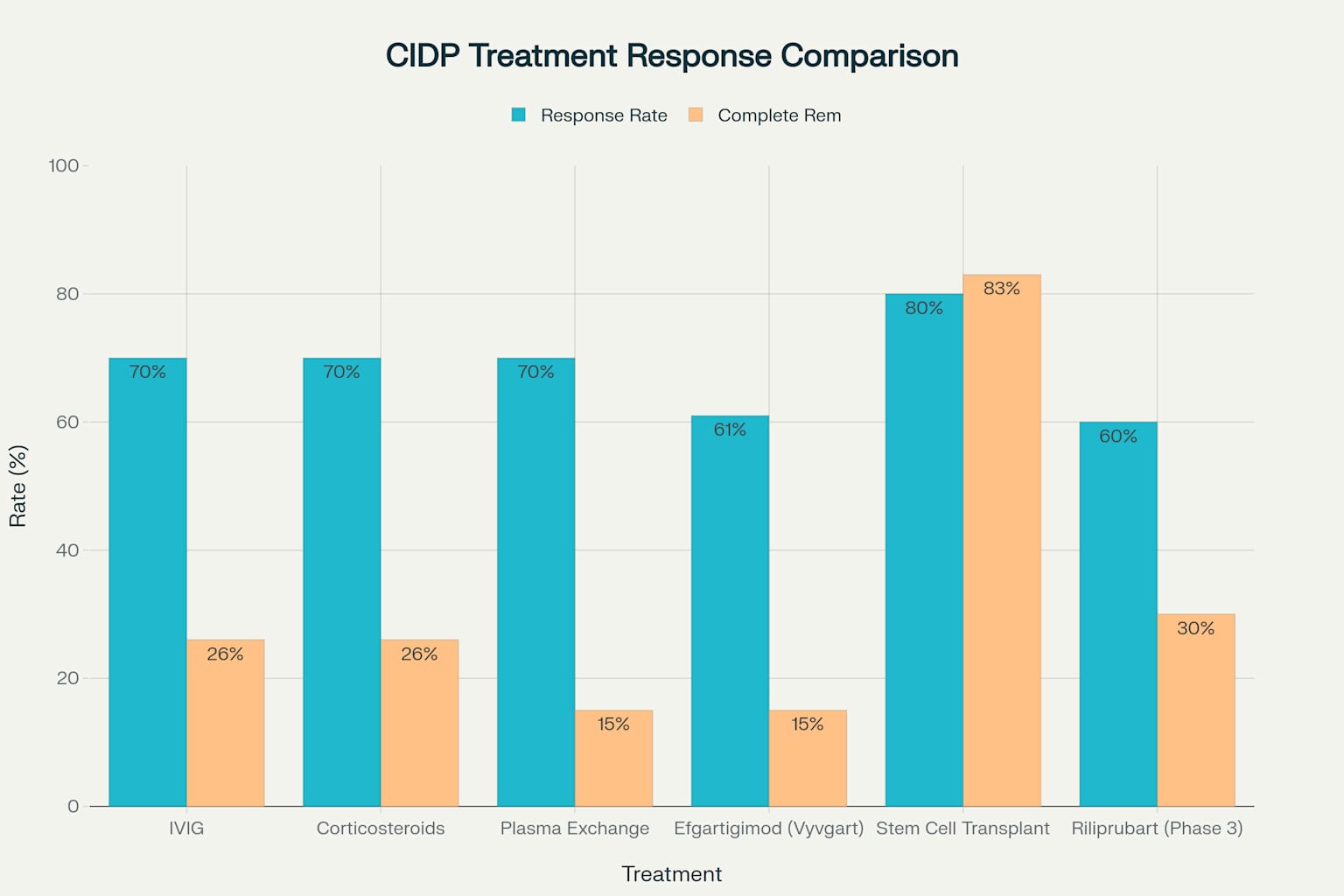
CIDP Treatment Response Rates: Understanding Your Options
Even more exciting developments are unfolding in clinical trials right now 1415. Sanofi's riliprubart is showing promising results in Phase 3 trials, with some patients experiencing sustained improvement for over a year 1516. What makes riliprubart special is that it's helping people who haven't responded well to standard treatments—a group that desperately needed new options 151617.
The Most Promising Path: Stem Cell Transplantation
Here's where the research gets truly exciting, though I want to be clear about the realities 18. Autologous hematopoietic stem cell transplantation—essentially resetting your immune system with your own stem cells—has shown the most dramatic results of any CIDP treatment 18.
In a major study following 60 CIDP patients who were dependent on IVIG or plasma exchange, stem cell transplantation achieved something remarkable: 83% were medication-free after five years, and 83% could walk without assistance 18. Before treatment, only 33% could walk unassisted 18. There were no treatment-related deaths 18.
The catch? It's still considered experimental, requires specialized centers, and involves significant risks 18. However, for people with severe, treatment-resistant CIDP, it represents genuine hope for what we might call a functional cure 18.
What the Research Tells Us About Recovery
The factors that predict better outcomes give us a roadmap for hope 5719. Early treatment makes an enormous difference — patients treated within months rather than years of symptom onset have significantly better long-term outcomes 4519.
Good response to your first treatment is one of the strongest predictors of long-term remission 5719. Younger age at diagnosis, symmetric symptoms (affecting both sides equally), and gradual rather than rapid onset all point toward better outcomes 57.
Perhaps most importantly, nerve conduction studies can now predict who's likely to respond well to treatment 19. Changes in specific nerve measurements within the first few months of treatment help doctors know if you're on the right track 19.
Looking Forward: The Pipeline of Hope
The next few years promise developments that edge us closer to that cure we're seeking 142021. Multiple new treatments are in late-stage trials, targeting different immune pathways than current therapies 141220.
Nipocalimab and batoclimab, two new FcRn blockers, are being tested in large trials with results expected by 2027 12. TAK-411, a completely different approach, begins Phase 2 trials this year 21. And complement inhibitors like riliprubart are showing that we can target the specific immune pathways driving CIDP damage 161722.
Perhaps most exciting is the growing understanding of CIDP biomarkers—blood tests that can predict treatment response and track disease activity 1723. Neurofilament light, a protein released when nerves are damaged, drops significantly with effective treatment and correlates with functional improvement 17.
The Reality of Living with Hope
I won't pretend that learning about remission rates and new treatments erases the grief of losing your pre-CIDP life 123. Jamilah, a CIDP patient whose story resonates with many of us, puts it perfectly: "Recovery is not linear," and society's expectation that medication will restore everything we've lost doesn't match the complex reality of autoimmune disease 124.
Therefore, here's what I've learned in my years with this condition and in researching these developments: while we may not have a cure in the traditional sense, we have something powerful — treatments that can stop progression, restore function, and in many cases, give us back our independence 4513.
For some, like the lawyer whose CIDP-related cognitive symptoms completely reversed with IVIG treatment, the improvement can feel miraculous 25. For others, it's a gradual return to activities that matter, supported by treatments that get better every year 29.
What This Means for You Today
If you're newly diagnosed, know this: early, aggressive treatment gives you the best shot at long-term remission 4519. Work with your neurologist to find the treatment that works for you, and don't give up if the first one doesn't deliver the results you're hoping for 513.
If you're treatment-resistant, new options are becoming available 111516. The approval of efgartigimod and the promising trial results for riliprubart mean that 2025 offers genuinely new hope for people who haven't responded to standard treatments 111516.
If you're somewhere in between—managing but not thriving—remember that CIDP research is moving faster than ever 2026. The treatments in development today could change the trajectory of your disease in ways we're just beginning to understand 202126.
While I can't promise you the instant, complete cure we all wish for, I can tell you this: the science is advancing, the treatment options are expanding, and the outlook for people with CIDP has never been brighter 4620. That may not be the cure we dreamed of, but it's the kind of hope that’s worth holding onto.
As always, consult with your neurologist about treatment options and never make changes to your therapy without medical supervision. The GBS/CIDP Foundation International remains our best resource for current treatment information and community support.

Neurojourney
📅 Closing Thoughts & How to Get Involved
Take advantage of these articles if you can, ask questions, and share what works for you. Together, we’re building a stronger, more informed CIDP community.
Want to support Cidpedia?
Share this article, consider a small donation, or send us your feedback. Every voice matters.
Stay strong, stay informed, and stay connected!
Warm regards,
Richard Aikman
Editor, CIDPedia
⚠️ Disclaimer
Let's get something important out in the open: WE ARE NOT DOCTORS and WE ARE NOT GIVING ADVICE! Everything we share comes from my personal journey living with CIDP, from research and from MY healthcare TEAM. While I've walked this path for a number of years, please remember: |
Cidpedia is an independent, patient-led newsletter. All information provided is for educational and informational purposes only and is not intended as medical advice, diagnosis, or treatment. We are not medical professionals. Always consult your physician or qualified health provider with any questions regarding your health or medical conditions. We respect your privacy and adhere to HIPAA guidelines when sharing stories or community contributions. All shared experiences are anonymized unless explicit permission is granted |
Stay strong, stay curious, and keep shuffling forward. 🌱

Reply